The Role of BiPAP Machines in Treating COPD
Chronic Obstructive Pulmonary Disease (COPD) is one of the leading causes of Breathing difficulties worldwide. For many, the challenge of simply getting enough air creates daily struggles. Traditional inhalers and oxygen therapy help, but when carbon dioxide builds up and Breathing becomes too taxing, BiPAP machines often step in as a critical part of treatment.
Who This Guide Is For and What You’ll Learn
This guide is designed for patients living with COPD, caregivers supporting loved ones, and individuals recently prescribed a BiPAP machine. By reading through, you will learn:
What BiPAP machines do and how they work.
When BiPAP helps people with COPD.
The benefits and risks of using BiPAP.
Practical tips for setup, comfort, and long-term use.
Quick Snapshot (TL;DR):
BiPAP machines support Breathing by pushing air in and out with alternating pressures, making it easier to clear carbon dioxide. They are invaluable during COPD flare-ups (exacerbations), in chronic respiratory failure, or at night when Breathing slows. Not everyone qualifies, but for those who do, BiPAP can reduce hospital visits, improve sleep, and prolong quality of life.
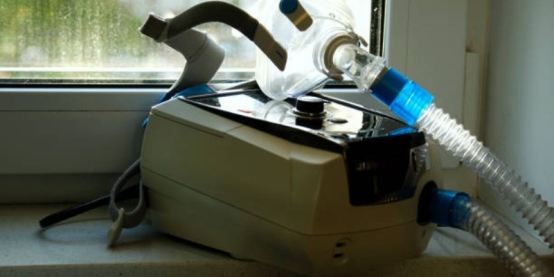
What is BiPAP and how it works
A BiPAP machine (Bilevel Positive Airway Pressure) delivers pressurised air through a mask. Unlike Continuous Positive Airway Pressure (CPAP)—which gives a single constant pressure—BiPAP alternates between:
IPAP (Inspiratory Positive Airway Pressure): Higher pressure to support inhaling.
EPAP (Expiratory Positive Airway Pressure): Lower pressure to make exhaling easier.
Some machines also have a backup rate, meaning if Breathing slows too much, the device triggers a breath. For COPD patients retaining carbon dioxide, this feature prevents dangerous buildup. By easing the work of Breathing, BiPAP allows fatigued lungs to rest and gases to rebalance.
When BiPAP is Used for COPD
Acute Situations
In hospital emergency rooms or ICUs, BiPAP is used during COPD exacerbations when patients:
Retain too much carbon dioxide (hypercapnia).
Develop respiratory acidosis (low blood pH from CO2 buildup).
Studies show BiPAP reduces the need for intubation, lowers mortality risk, and shortens hospital stays.
Chronic or Long-Term Use
For stable COPD patients, BiPAP is considered when:
There’s long-term carbon dioxide retention.
Symptoms include frequent morning headaches, sleepiness, and worsening breathlessness.
Overlap conditions are present, such as sleep apnea and COPD together.
BiPAP at home can be life-changing, though it is not suitable for everyone. Contraindications include facial injuries, unstable blood pressure, or inability to manage the airway independently.
Do You Need BiPAP? Candidacy Checklist
Doctors consider both symptoms and test results, such as:
Symptoms: morning headaches, fatigue, daytime sleepiness, frequent flare-ups, worsening shortness of breath.
Tests: high PaCO₂ on arterial blood gas, oxygen levels during sleep studies, and oximetry patterns.
Conditions: obesity, hypoventilation, obstructive sleep apnea, or heart failure often strengthen the case.
If breathlessness is severe, or confusion and cyanosis develop, urgent evaluation is needed.
BiPAP vs CPAP for COPD
When CPAP is enough: Pure sleep apnea without carbon dioxide retention.
When BiPAP is better: COPD patients with hypercapnia who need active pressure support for inhalation and exhalation.
Advanced BiPAP modes such as ST (spontaneous-timed) or AVAPS/iVAPS target ventilation volumes for more complex cases.

Expected Benefits and Realistic Outcomes
Short-term benefits: Less breathlessness, better sleep, improved gas exchange.
Long-term benefits: Fewer hospitalisations, better quality of life, and possibly survival benefits for selected patients.
However, success depends heavily on consistent nightly use, correct settings, and addressing comorbidities.
Risks, Side Effects, and Prevention
Common issues: dryness, bloating (aerophagia), mask discomfort, and claustrophobia.
Less common: aspiration, hypotension, and rare barotrauma.
Prevention tips:
Use humidification and heated tubing for dryness.
Try different masks for a better fit and comfort.
Seek medical advice if headaches, confusion, or worsening breathlessness occur.
Getting Started with BiPAP
To begin therapy, evaluation by a pulmonologist is required. This includes lung testing and sometimes a sleep study. BiPAP prescriptions outline starting pressure ranges and whether oxygen needs to be integrated.
During the first week, compliance strategies include gradually wearing the mask longer each night, adjusting humidity, and ensuring proper mask fit. Oxygen can be blended safely with BiPAP under medical guidance, keeping COPD patients within target SpO₂ ranges recommended by the American Lung Association.
Masks and Comfort: Making It Work
Types of masks include nasal masks, nasal pillows, and full-face masks.
Leaks can be reduced by using liners, proper straps, and a full-face model if mouth Breathing occurs.
Comfort options include heated humidity and gradual desensitisation for claustrophobia.
Living with BiPAP at Home
Day-to-day success depends on consistent cleaning, replacing worn-out cushions, and adapting to lifestyle needs:
Backup power for outages.
Travel planning with documentation and power adapters.
Hygiene practices to prevent infections.
Optimising Therapy: Monitoring and Adjustments
Modern BiPAP devices track usage hours, tidal volume, and leaks. Telemonitoring allows providers to adjust settings remotely.
Quick Troubleshooting:
Dryness: increase humidifier settings.
Leaks: Try alternative masks or adjust pressure levels.
Bloating (aerophagia): lower inspiratory pressure.
If symptoms persist, advanced mode changes may be necessary.
Costs, Insurance, and Access
BiPAP machines are often covered under insurance, either fully or partially, when specific test results support use. Out-of-pocket costs can be significant, especially for masks and replacement parts. Patients should request training sessions and complete explanations from their equipment provider. Low-cost access may be available through healthcare programs listed at Medicare.gov.
Brands, Models, and Features That Matter
Key features that support COPD patients include:
Adjustable backup rate and broad pressure support ranges.
Integrated oxygen ports.
Noise level and ease of monitoring.
Machines differ in terms of interface options, portability, noise reduction, and monitoring abilities.
Alternatives and Complements to BiPAP
High-flow nasal cannula: another hospital treatment option.
Long-term oxygen therapy: still vital for some COPD patients.
Lifestyle interventions: pulmonary rehabilitation, smoking cessation, and proper nutrition support. Breathing long-term.

Safety and Emergency Guidance
COPD patients should maintain oxygen targets within safe ranges to avoid suppression of Breathing drive. Emergency care is required if confusion, cyanosis, or inability to clear secretions develops. An action plan coordinated with the healthcare team ensures confidence in these scenarios.
Caregiver Corner
Caregivers play a central role in adjusting masks, cleaning equipment, and recognising warning signs. Early recognition of morning headaches, rising confusion, and worsening breathlessness can prevent emergencies.
Myths and Misconceptions
BiPAP isn’t only for sleep apnea—it is essential in COPD.
More oxygen is not always better; overuse can trigger dangerous CO₂ rises.
Starting BiPAP doesn’t always mean lifelong dependence.
It’s not just for the “end stage” but can provide earlier relief.
Getting Help for COPD with BiPAP
Living with COPD is difficult, but for many patients, BiPAP provides critical relief. With proper evaluation, setup, and ongoing support, BiPAP machines empower patients to breathe easier, stay out of the hospital, and focus on daily life with greater comfort.